My DCISionRT Test Results: A Radiation Reflection Five Years in the Making
A Sponsored Post with PreludeDX
I was diagnosed with DCIS in 2019 at age 41 and chose a lumpectomy followed by radiation. With the information I had during my decision-making process, radiation made sense. At the time, I didn’t know about DCISionRT.
I had no idea there was a test that would help me understand my personal benefit from radiation. I began learning about the test in mid-2020 and was intrigued. I’ve often wondered what it would have told me and how it would have impacted my radiation decision.
In 2024, I began a patient advocacy relationship with PreludeDX to support and encourage breast cancer patients. Imagine my surprise when they mentioned that they would be willing to run DCISionRT on my DCIS sample so I could see my results.
It wouldn’t change my radiation decision- because I completed the treatment- but it would allow me to write and reflect on my results.
I’ve written about how making cancer decisions often feels like we are attempting to put together a puzzle without all the pieces on the table. I remember feeling anxious every time a new piece of information showed up. Would this new information add or subtract to my overall treatment plan?
So now, I have a new piece to my DCIS decision-making puzzle. What does it tell me?
Disclaimer: I am not a doctor, and I’m not sharing medical advice here. Please consult your medical team for all of your medical questions.
What is DCISionRT?
Before sharing my DCISionRT results, I thought I’d explain a little about what DCISionRT is. If you’d like to learn more about their test and the study results backing it up, please check out their website here.
DCISionRT helps DCIS patients make radiation treatment decisions. The test can be run on a core needle biopsy result or a tumor sample after surgery. In my case, it was run on a sample of my DCIS that had been removed in 2019 and stored in the pathology lab.
DCISionRT assesses 10-year recurrence risk and predicts radiation benefits after breast-conserving surgery. It uses a combination of multi-biomarker expression (such as HER2 and Ki-67) and clinicopathologic features (size of tumor, margin status, patient age) to calculate an individualized DCISionRT score for patients diagnosed with DCIS.
More information about biomarker tests and breast cancer can be found here.
DCISionRT is a biomarker test designed specifically for DCIS to help patients and their medical teams make shared radiation treatment decisions. Patients receive a numerical score to help them understand the potential benefit from radiation and their recurrence risk with and without radiation. Whether or not a patient decides to take endocrine therapy is not a factor in the DCISionRT results.
What were my DCISionRT Results?
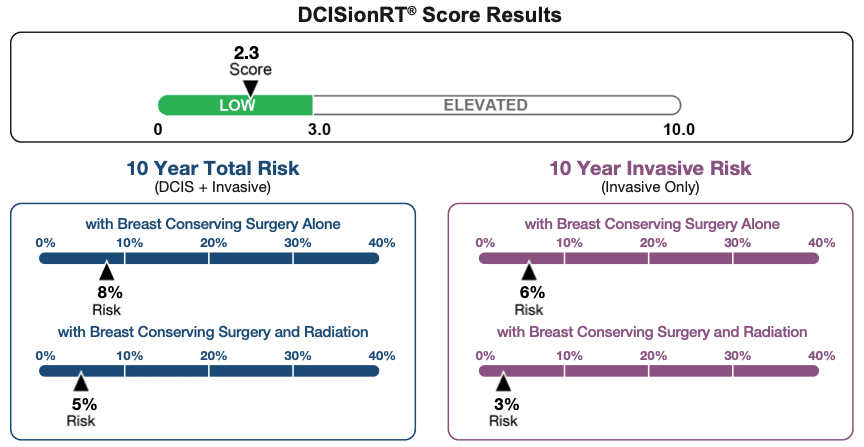
As you can see, my DCISionRT score fell into the low side of the scoring range. I scored a 2.3 out of 10. This means that in the eyes of the test, I fall into the category of patients who receive a lower benefit from radiation.
This isn’t surprising to me. I knew that my DCIS was low grade, small, and removed with clean margins. Additionally, I tested negative with my genetic tests.
What was encouraging was that radiation did lower my risk of recurrence. It wasn’t a huge number, but it is significant to me. I’m now five years into my survivorship, and I hope to have many more years without a recurrence.
According to my DCISionRT results, with surgery alone, my 10-year risk of recurrence of either DCIS or Invasive cancer in the same breast was 8%. With radiation, my risk of recurrence drops to 5%.
So, by doing surgery and radiation, I reduced my risk of getting another breast cancer in my right breast down to 5%. Additionally, my treatment choice moved my risk of invasive breast cancer from 6% to 3% in that breast.
As I wrote above, these results don’t factor in tamoxifen or other endocrine therapies. This gives even more peace of mind. I began taking tamoxifen in early 2020 and was unable to stay on the medication for the full five years due to side effects (you can read about it here).
Reflections on my DCISionRT Results
While I can’t go back in time with a time machine and see these results in 2019, before I made my radiation decision, I can share a few of my current reflections. I’m writing this a few weeks after I received my results, and I’ve been thinking a lot about their impact.
I’m still glad I did radiation. These results show that radiation reduced my risk of recurrence. My risk of recurrence was low, to begin with, and radiation lowered it even further.
When I was making my treatment decisions, I wanted to choose the most effective treatments for the DCIS I had. I also didn’t want to do more surgery than required for this small cancer. While I could have chosen a mastectomy and avoided radiation and additional screenings, that didn’t align with my goals.
I had the option of breast-conserving surgery for this cancer, and my surgeon was confident he could remove it and preserve the cosmetic appearance of my breast along the way. That is exactly what happened. I have a small scar and no change to my breast shape.
I was 41 at diagnosis, so radiation was highly recommended. In addition, I wanted to do everything in my power to treat the cancer and then get back to life.
Radiation lowered my recurrence risk- and my DCISionRT results show that. For me, it didn’t cut the risk in half as is often quoted, but it did drop it by three percentage points. Those three percentage points feel significant to me, especially knowing where I was in my life at the time of diagnosis with school-aged kids.
So, what would I do if I had a DCIS diagnosis again?
I would ask for DCISionRT to be run on my core needle biopsy results to help me make my decisions. It is possible that my 2019 experience with DCIS may not be my only journey with breast cancer. I hope it is, but there is no guarantee.
If the DCIS were in my right breast, re-radiation likely isn’t an option. But, if my sample were low risk, maybe I would opt for surgery alone.
If the DCIS were in my left breast (the one that didn’t have DCIS before), then I would need to consider if it was worth it to me to go through more radiation. Radiation was difficult for me to endure. The fatigue and the skin peeling were significant. I didn’t breeze through it.
Because I went straight from surgery to radiation within a few weeks, I didn’t have an accurate picture of the impact of radiation on my recovery until a few years later.
In 2022, I had a lumpectomy to remove a suspicious lesion on my left breast. The biopsy results had been inconclusive, so the treatment recommendation was to remove it. Thankfully, it was benign. I recovered very quickly from the surgery. In a few weeks, I was back to all my normal activities. Surgery without radiation was much easier to recover from!
After experiencing the difference in recovery, it makes me even more likely to use DCISionRT if I ever have another DCIS diagnosis. Radiation was hard, and if I could safely skip it, I would. DCISionRT offered me a window into my DCIS that I didn’t have before. I’m grateful to have been able to add another piece to my DCIS puzzle (even if it came a few years after the fact).
Sponsored Post: This is a sponsored post as part of my patient advocacy relationship with PreludeDX. They provided the DCISionRT test at no cost to me and asked me to write my reflections here. The information in this post reflects my opinions and should not be considered medical advice.
This article has also been published on PreludeDX’s website.
Jennifer Douglas
Jennifer Douglas is an author, patient advocate, and DCIS breast cancer survivor. After navigating her own breast cancer journey in 2019, she began writing and encouraging others who were newly diagnosed. Her resources include her book, "A Breast Cancer Journey: Living It One Step at a Time," and her online support course, "Encourage: Breast Cancer and Beyond." Jennifer also actively supports patients through her online presence and direct involvement in communities and support groups, offering guidance and encouragement every step of the way.


You May Also Like

HealthGrades Post: Breast Cancer- A Life Pivot I Wasn’t Expecting
August 8, 2022
Vaginal Estrogen: Low Dose, High Impact
August 31, 2024